RGUHS Nat. J. Pub. Heal. Sci Vol No: 10 Issue No: 4 eISSN: 2584-0460
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Department of Community Medicine, Koppal Institute of Medical Sciences, Koppal, Karnataka, India
2Department of Community Medicine, Karnataka Medical College and Research Institute, Hubballi, Karnataka, India
3Department of Community Medicine, Koppal Institute of Medical Sciences, Koppal, Karnataka, India
4Dr. Sharankumar Holyachi, Assistant Professor, Department of Community Medicine, Koppal Institute of Medical Sciences, Koppal, Karnataka, India.
5Department of Community Medicine, Jawaharlal Nehru Medical College, KLE University of Higher Education and Research (KAHER), Belagavi, Karnataka, India
*Corresponding Author:
Dr. Sharankumar Holyachi, Assistant Professor, Department of Community Medicine, Koppal Institute of Medical Sciences, Koppal, Karnataka, India., Email: sharanholyachi2010@gmail.com
Abstract
Background: Diabetes mellitus (DM) is a chronic metabolic disorder characterized by high blood glucose levels resulting from insufficient insulin production or impaired insulin action. Effective management of diabetes requires consistent healthcare engagement, appropriate lifestyle modifications, and adherence to prescribed treatments. Inadequate treatment and inappropriate health-seeking behaviors (HSB) among individuals with diabetes mellitus can lead to severe, potentially life-threatening complications, and increased mortality.
Objectives: To determine the HSB pattern and associated factors among individuals with known type 2 diabetes mellitus attending health training facilities in both rural and urban areas.
Methods: This cross-sectional study was conducted for a period of six months among known cases of type 2 diabetes attending urban and rural health centers. Convenient sampling was used to recruit the study participants, 200 each from rural and urban areas. Data were collected using a semi-structured questionnaire and entered in Microsoft Excel 2010, and statistical analysis was performed using IBM SPSS v.25.
Results: The majority of participants were aged above 50 years. Diabetes was diagnosed in government-run healthcare facilities for 70% of the respondents, and 36.8% underwent routine screening and continued to seek care at these facilities. Most participants (93.5%) were on oral anti-diabetic medications. Participant location and health insurance enrollment were found to be significant determinants of appropriate health-seeking behaviour.
Conclusion: The study population demonstrated high level of appropriate HSB, with the majority relying on government healthcare facilities for the diagnosis and management of diabetes mellitus.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by high blood glucose levels due to insufficient insulin production or ineffective insulin action.1 It is a significant global health concern, leading to complications such as cardiovascular diseases, kidney failure, nerve damage, and vision impairment.2 The global diabetic population is projected to reach 1.3 billion by 2050, with every country expected to experience an increase in cases.3
According to the International Diabetes Federation (IDF) Diabetes Atlas (2021), India has approximately 77 million people living with type 2 diabetes mellitus and an estimated 25 million are pre-diabetic. Alarmingly, more than 50% of diabetics are unaware of their condition, leading to late diagnosis and increased risk of complications.4,5
The escalating prevalence of diabetes poses substantial challenges to healthcare systems globally. Addressing this epidemic requires comprehensive strategies focusing on prevention, early diagnosis, and equitable access to effective treatments. The World Health Organization emphasizes the urgent need for stronger global action to address rising diabetes rates and widening treatment gaps, particularly in low-middle income countries.6
In the study, appropriate health-seeking behaviour (HSB) is defined as seeking modern treatment, either oral hypoglycemics or insulin injections, from government or private health facilities, with adherence to treatment and regular follow-up visits.7 Understanding HSB in individuals with diabetes is crucial for improving disease outcomes and reducing complications.8 Managing diabetes requires consistent healthcare engagement, lifestyle modifications, and adherence to medical treatment.9 Inadequate treatments and inappropriate HSB in individuals with diabetes mellitus can lead to life-threatening complications and increased mortality.
In India, HSB among diabetes mellitus patients is influenced by a complex interplay of socioeconomic, cultural, and healthcare system factors.10 Understanding these determinants is crucial for developing effective interventions to improve diabetes management and outcomes. Addressing these multifaceted challenges requires a comprehensive approach that includes enhancing public awareness, improving healthcare accessibility, integrating traditional and modern medical practices, and implementing supportive policies to alleviate the economic burden on patients.11
Considering the increasing burden of diabetes in India, driven by rapid urbanization and sedentary lifestyles, the HSB among diabetics remains poorly characterized in both rural and urban areas. The limited number of studies conducted in this area to determine the HSB patterns and associated factors highlights the need for undertaking the present research.
Materials and Methods
This cross-sectional study was conducted over a six-month period at the rural and urban heath training centers of a medical college in Karnataka, India. The rural health training center is located 18 km from the city and serves a population of approximately 21,000, while the urban center is located within the city and covers a population of about 79,000. Medical postgraduate students and intern trainees are posted at both centers to provide healthcare services to the community. Both centers regularly screen and manage non-communicable diseases. Monitoring of blood glucose levels is performed monthly using a glucometer during follow-up visits, in accordance with the National Program for Prevention and Control of Non-Communicable Diseases (NP-NCD). Institutional Ethics Committee approval was obtained for the study, and permission to conduct the study was secured from the administrative medical officers of the respective health centers.
The sample size was calculated using the formula I2/ I2, with confidence level (Z-1.96). The prevalence of diabetes in Karnataka, as reported in the National Family Health Survey-5 (2019-2021), is 14%.12 Considering this prevalence, with an allowable error of 3.7% and a 10% non-response rate, the final sample size was estimated to be to 400. Convenient sampling was employed to recruit the study participants, with 200 individuals selected each from the rural and urban areas. After establishing rapport, written informed consent was obtained from all participants. For those who were illiterate, the investigator read out the consent form in local language (Kannada). Once their understanding and willingness to participate were confirmed, a thumb impression was taken on the consent form printed in Kannada. A predesigned, semi-structured questionnaire was used to collect information related to identification details and socio-demographic characteristics of the study participants.
Participants aged above 30 years, who were known cases of type 2 diabetes mellitus, residing in the study area for more than six months, and willing to provide written informed consent were included in the study. Subjects with impairment of speech, hearing, or cognition were excluded.
The current study adopted the definition of appropriate health-seeking behaviour (HSB) from previously published literature, wherein HSB is defined as seeking modern treatment, either oral hypoglycemics or insulin injections, from government or private health facilities,with adherence to treatment and regular follow-up visits.7
Data on the determinants of HSB were collected through direct interviews using a structured medical questionnaire. The determinants assessed included age, gender, place of residence (rural/urban), type of family, educational status, socioeconomic status, place of diagnosis, duration of disease, presence of comorbidities, family history of diabetes mellitus, health insurance coverage, smoking status, and alcohol consumption.
Statistical Analysis
Data were collected through face-to-face interviews using a semi-structured questionnaire. The collected information was entered into Microsoft Excel 2010 and analyzed using IBM SPSS v.25.0 software. Descriptive statistics such as frequencies, percentages were applied. Baseline characteristics were analyzed using the χ2 test for nominal variables, while continuous variables were expressed as median (IQR). Univariate and multivariate logistic regression methods were used to analyze the association between various determinants and appropriate HSB. Results were presented in tables and pie charts. All P values were based on two-sided tests, and a P value of <0.05 was considered statistically significant.
Results
Among the 400 participants, the majority were aged above 50 years (74.2%), with nearly equal representation of females (50.2%) and males (49.8%). Most participants were Hindus (79.5%), living in nuclear families (57.8%), and were married (95.5%). Nearly half of the respondents were illiterate (49%), with 39.5% being manual labourers by occupation. The majority belonged to the lower-middle socioeconomic class, as per the Modified B.G. Prasad Classification (January 2024) (Table 1)
A family history of diabetes was present in 36.3% of the participants, and 42% reported comorbid conditions. Hypertension was the most common comorbidity, accounting for 71% of these cases. Over half of the respondents (51.7%) had been diagnosed with diabetes mellitus for five years. The majority (79.1%) initiated treatment immediately after diagnosis. The major reason cited for delay in seeking treatment was the perception that their symptoms were not serious enough to require medical care (Tables 2 and 3).
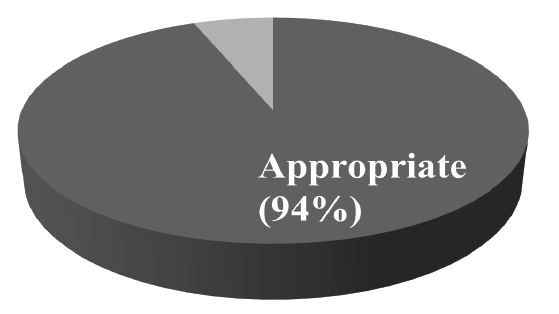
Ninty-four percent of the participants demonstrated appropriate health-seeking behaviour. They were receiving oral hypoglycemic agents or insulin injections from government or private health facilities, adhering to treatment, and attending regular follow-up visits (Figure 1).
Diabetes mellitus was diagnosed at government health facilities for 70% of the respondents, with 36.8% being identified during routine screenings at healthcare centers. Most respondents (93.5%) reported using government health facilities to obtain oral hypoglycemic agents. Health insurance coverage was availed by 29.8% of respondents (Table 4).
Associations between HSB and various parameters were analyzed using a logistic regression model. A highest proportion of respondents aged below 50 years, as well as females, demonstrated appropriate HSB. Respondents belonging to the upper socioeconomic also showed better HSB compared to those from lower socioeconomic classes. In the univariate analysis, place of residence (rural/urban) and health insurance coverage were significantly associated with appropriate HSB (Table 5). Rural residents exhibited better HSB than urban residents.
The logistic regression analysis showed that adjusted odds ratios for participant’s location [0.205 (0.068- 0.618)] and health insurance enrollment [8.837 (1.169- 9.678)] were statistically significant determinants of appropriate HSB.
Discussion
In this cross-sectional study, multiple parameters were analyzed to assess their association with appropriate HSB. The findings indicated that place of residence and health insurance coverage were significantly associated with appropriate HSB.
Age Factor in HSB
Different age groups often face varying health concerns, preferences, and barriers when seeking medical care. Younger patients often exhibit inadequate health information-seeking behavior, contributing to poor glycemic control and a higher prevalence of complications.13 In contrast, older adults generally possess greater knowledge about diabetes, which is positively associated with proactive health-seeking behavior and improved disease management.14 In the present study, most participants (74%) were aged above 50 years. However, univariate analysis did not show a statistically significant association between age and appropriate HSB.
Gender Differences in HSB
Gender plays a crucial role in HSB, influencing how individuals perceive illness, access to healthcare, and adherence to treatment.15 Societal norms, cultural ex-pectations, economic factors, and biological differences contribute to distinct health-seeking patterns among men and women.16 Men commonly delay seeking medical attention until symptoms become severe, whereas women tend to utilize healthcare services more frequently, particularly for reproductive, maternal, and chronic health needs.17,18 In the present study, females demonstrated better HSB compared to males; however, this difference was not statistically significant.17 This may be attributed to improved accessibility and availability of healthcare services in the study area.
Financial Constraints and HSB
Many patients, especially in rural and low-income urban areas, face financial difficulties that hinder regular follow-ups and consistent medication adherence. High costs of medications, diagnostics, and insulin therapy often deter individuals from seeking timely care.19 A cross-sectional study conducted in Jaipur, Rajasthan, reported that financial constraints significantly affect access to healthcare services and adherence to treatment, emphasizing the need for more affordable healthcare strategies to alleviate the economic burden on patients.20
In the present study, participants from the upper socioeconomic class exhibited better HSB than those belonging to lower socioeconomic classes; however, this difference was not statistically significant. This may be due to the larger proportion of participants belonging to lower socioeconomic groups. It indicates that the burden of diabetes is increasing among economically disadvantaged sections of society, highlighting the need to revise diabetes management strategies and reduce out-of-pocket expenditure in the long term. Government schemes such as Ayushman Bharat in India aim to make diabetes treatment more accessible and affordable.21
Educational Barriers in HSB
Limited health literacy can lead to poor understanding of diabetes symptoms, complications, and the importance of early medical intervention. In the present study, no significant difference in HSB was observed between literate and illiterate participants. However, multiple studies have reported that income level and education significantly influence HSB among diabetic patients. A study by Huang et al., found that individuals with higher education levels were more likely to seek timely medical attention and adhere to treatment plans.22 A study conducted in rural Guangxi, China, reported that patients with better diabetes-related knowledge were more proactive in seeking health information and managing their condition.23 Lower education status often results in reduced awareness and fewer opportunities to adopt preventive measures and appropriate HSB.
Access to Care in HSB
In the present study, the rural-urban difference in HSB was found to statistically significant. Rural regions often lack specialized healthcare providers, making it challenging for patients to receive optimal diabetes management. Studies highlight that rural populations have limited access to specialized diabetes care, leading to delayed diagnosis and inadequate management.24
Health Insurance and HSB
The expenses associated with diabetes care, including medications and diagnostic tests, pose a significant burden, particularly on uninsured individuals. Health insurance coverage has been positively correlated with better HSB, as it reduces the financial burden associated with diabetes management.25 In the present study, 29.8% of participants were enrolled in health insurance schemes and a statistical significant association was noted between health insurance coverage and appropriate health-seeking behaviour. A study conducted in Mangalore identified several obstacles to treatment compliance among diabetic patients, including financial difficulties. These barriers often led to delayed healthcare seeking and poor disease management.26 Increasing awareness and enrollment in health insurance schemes is essential to reduce out-of-pocket expenditure.
Impact of Disease Severity on HSB
The severity of a disease significantly influences how and when individuals seek healthcare. People with mild symptoms often delay or avoid seeking medical attention, while those experiencing severe or life-threatening conditions are more likely to seek urgent care. In the present study, ‘perceiving symptoms as not serious enough for treatment’ was the primary reason for inappropriate HSB among 47% of participants. Previous studies have similarly reported that being symptomatically normal or not serious were predominant reasons for not seeking healthcare.27
Duration of Disease and HSB
The median duration of diabetes reported in the previous studies ranged between 5 and 8 years.21,28 In the present study, the median duration was 5 years. However, the duration of diabetes did not show a statistically significant association with appropriate HSB.
Presence of Comorbidity and HSB
In the present study, 42% of respondents reported comorbidities, the commonest being hypertension (71%). The presence of comorbid conditions did not show statistically significant association with appropriate HSB. A study by Bhosale et al. reported that 69.6% of participants had diabetes-related comorbidities.29 Greater attention must be given to individuals with comorbidities to prevent early complications and disabilities, emphasizing the need for appropriate HSB in this group.
Family History and HSB
The odds of regular follow-up were found to be higher among individuals with a family history of diabetes mellitus.28 In the present study, 36.3% of participants had a family history of diabetes; however, this did not show a statistically significant association with HSB. Studies conducted in different regions of India have reiterated the influence of family history on HSB.29,30 Preventive and promotive health activities, like adopting a healthy diet, engaging in regular physical activity, and maintaining a healthy lifestyle, can minimize the hereditary impact on diabetes-related complications.
Smoking and Alcohol Habits on HSB
In the present study, the prevalence of smoking (30%) and alcohol use (12%) was comparatively low. Previous research from Nepal reported that non-smokers demonstrated better follow-up care.28 These findings collectively emphasize the critical role of addressing smoking and alcohol consumption in the management of diabetes. Healthcare providers should prioritize interventions that support cessation of smoking and moderation of alcohol intake to improve health outcomes and encourage proactive HSB among individuals with diabetes.
Conclusion
The study revealed that a majority of the population demonstrated appropriate HSB (94%), as most participants were on regular medications, undergoing periodic blood investigations, following advised dietary modifications, and were satisfied with their health status. A large proportion of respondents depended on government health facilities for treatment, emphasizing the importance of strengthening public healthcare infrastructure. The present study underscores the multifaceted nature of HSB among diabetes patients, influenced by socioeconomic status, education, and place of residence. Understanding these determinants is crucial for developing targeted interventions that promote timely and effective healthcare utilization among individuals with diabetes.
Limitations
This study was restricted to participants within the administrative limits of training centers of a medical college. HSB is influenced by complex socio-cultural, demographic, and economic factors. Therefore, conducting further research activities involving diverse population groups will enhance knowledge base on HSB. The current study intended to assess the health-seeking behaviour among known cases of type 2 diabetes mellitus; however, evaluating the impact of disease severity could have provided additional insight.
Recommendations
The socio-cultural influences of HSB among patients with diabetes mellitus require focused attention, especially in rural areas. Since the majority of the participants relied on government health institutions for diagnosis and follow-up care, strengthening the healthcare infra-structure, improving capability of healthcare personnel, and fostering trust in public health services are essential.
Ethics approval: The study was approved by Institutional Ethics Committee of Koppal Institute of Medical Sciences, Koppal (KIMS-KOPPAL/IEC/167/2023-24)
Conflicts of Interest
There are no conflicts of interest
Financial Support
Nil
Acknowledgement
Authors would like to acknowledge all the study participants for their co-operation and providing requisite information for the study. We also acknowledge the Medical Officers of both the health centers for their administrative support and guidance.
Supporting File
References
1. World Health Organization. Diabetes [Internet]. World Health Organization. Geneva: WHO; 2024. Available from: https://www.who.int/news-room/ fact-sheets/detail/diabetes
2. International Diabetes Federation (IDF). IDF Diabetes Atlas. 10th ed. Brussels: International Diabetes Federation; 2021.
3. Institute for Health Metrics and Evaluation. Global diabetes cases to soar from 529 million to 1.3 billion by 2050 [Internet]. Seattle (WA): IHME; 2023. Available from: https://www.healthdata.org/news-events/newsroom/news-releases/global-diabetes-cases-soar-529-million-13-billion-2050
4. International Diabetes Federation. India: Diabetes country report 2000-2045 [Internet]. Brussels: IDF; 2021. Available from: https://diabetesatlas.org/data/ en/country/93/in.html
5. World Health Organization. Diabetes India [Internet]. New Delhi: WHO; [cited 2026 March 5]. Available from: https://www.who.int/india/ health-topics/diabetes
6. World Health Organization. Urgent action needed as global diabetes cases increase four-fold over past decades [Internet]. Geneva: WHO; 2024. Available from: https://www.who.int/news/item/13-11-2024- urgent-action-needed-as-global-diabetes-cases-increase-four-fold-over-past-decades
7. Thapa S, Jha N, Baral DD, et al. Healthcare seeking behaviour among people living with type 2 diabetes in rural area of Eastern Nepal. Int J Pub Health Safe 2018;3:166.
8. Bosnjak M, Ajzen I, Schmidt P. The theory of planned behavior: Selected recent advances and applications. Eur J Psychol 2020;16(3):352-356.
9. World Health Organization. Diabetes [Internet]. Geneva: WHO; 2024. Available from: https://www. who.int/news-room/fact-sheets/detail/diabetes
10. Dey S, Mukherjee A, Pati MK, et al. Socio-demographic, behavioural and clinical factors influencing control of diabetes and hypertension in urban Mysore, South India: a mixed-method study conducted in 2018. Arch Public Health 2022;80(1):234.
11. Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: A scientific review. Diabetes Care 2020;44(1):258-79.
12. International Institute of Population Sciences, ICF. National Family Health Survey (NFHS-5), 2019- 21: India. Mumbai: IIPS; 2021.
13. Wang Y, Zhang Y, Guo T, et al. Knowledge level and health information-seeking behavior of people with diabetes in rural areas: a multicenter cross-sectional study. Front Public Health 2024;12:1285114.
14. Abidin SIZ, Sutan R, Shamsuddin K. Prevalence and determinants of appropriate health seeking behaviour among known diabetics: results from a community-based survey. Advances in Epidemiolo-gy 2014;2014:793286.
15. Ballering AV, Olde Hartman TC, Verheij R, et al. Sex and gender differences in primary care help-seeking for common somatic symptoms: a long-
itudinal study. Scand J Prim Health Care 2023;41 (2):132-139.
16. Thompson AE, Anisimowicz Y, Miedema B, et al. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract 2016;17:38.
17. Jackson MC, Dai S, Skeete RA, et al. An examination of gender differences in the national diabetes prevention program's lifestyle change program. Dia-betes Educ 2020;46(6):580-586.
18. Siddiqui MA, Khan MF, Carline TE. Gender differences in living with diabetes mellitus. Mater Sociomed 2013;25(2):140-2.
19. World Health Organization. Evidence for action [Internet]. Geneva: WHO; 2003. Available from: https://iris.who.int/bitstream/ handle/10665/42682/9241545992.pdf
20. Datta B, Datta BC, Dubey S, et al. Health-seeking behavior and economic burden of patients with type 2 diabetes mellitus: a cross-sectional study. Cureus 2024;16(10):e70806.
21. Press Information Bureau. Steps taken by Government to support diabetes patients [Internet]. New Delhi: PIB; [[cited 2026 March 5]. Available from: https://pib.gov.in/PressReleaseIframePage.aspx- ?PRID=1882179
22. Chawla SPS, Kaur S, Bharti A, et al. Impact of health education on knowledge, attitude, practices and glycemic control in type 2 diabetes mellitus. J Family Med Prim Care 2019;8(1):261-268.
23. Wang Y, Zhang Y, Guo T, et al. Knowledge level and health information-seeking behavior of people with diabetes in rural areas: a multicenter cross-sectional study. Front Public Health 2024;12:1285114.
24. Gupta SK, Lakshmi P, Chakrapani V, et al. Understanding the diabetes self-care behaviour in rural areas: Perspective of patients with type 2 diabetes mellitus and healthcare professionals. PLoS One 2024;19(2):e0297132.
25. Casagrande SS, Park J, Herman WH, et al. Health insurance and diabetes. In: Lawrence JM, Casagrande SS, Herman WH, et al., editors. Diabetes in America [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); 2023.
26. Mentock SM, Ng VY, Narayana R, et al. Treatment-seeking behavior and obstacles to treatment compliance in diabetic patients in Mangaluru, India. Diabetes Metab Syndr 2017;11Suppl 2:S617-S622.
27. Kishore J, Kohli C, Gupta N, et al. Awareness, practices and treatment seeking behavior of type 2 diabetes mellitus patients in Delhi. Ann Med Health Sci Res 2015;5(4):266-73.
28. Silvanus V, Maharjan S, Jha A. Factors influencing health seeking behaviour among persons with diabetes attending urban health care settings. J Nepal Health Res Counc 2022;20(2):347-353.
29. Bhosale S, Pawar AT, Kumar KD. Health care-seeking behavior among diabetic patients in Kozhikode, Kerala. Int J Med Sci Public Health 2017;6(10):1524-1527.
30. Savitha Rani BB, Kulkarni P, Ashok NC, et al. Assessment of health seeking behaviour of type ii diabetes patients attending tertiary care centre at Mysuru: A concern and call for action. Indian Journal of Preventive Medicine 2018;6(2):99-105.